A discussion about vasectomy is likely to cause grown men to cringe, cross their legs, and ball up in a fetal position. Many men who enter my office reveal that they are only there because their wife forced them to come. Frequently their friends and co-workers have filled their minds with stories (some of them fictitious) about vasectomy and the recovery. So sit back and relax while you learn the truth about vasectomy.
FACT: Compared to female sterilization, vasectomy is more effective, less expensive, and has fewer complications.¹
Vasectomy is performed under local anesthesia, and often with a mild sedative. Before vasectomy, a physical examination (with emphasis on testicular or other scrotal abnormalities) should be performed to rule out testicular cancer or other disease.
Vasectomy usually takes 20-30 minutes to perform. During the procedure, the structure called the vas deferens is closed. There is a vas deferens on each side of the scrotum (Figure 1). This muscular tube has a diameter somewhere between a spaghetti noodle and a cell phone charging cord. Its only function is to propel mature sperm toward the prostate and urethra for ejaculation.
Access to these tubes is usually through a single ½ inch opening in the upper scrotum. This is usually done via a non-scalpel approach. This means that a sharpened instrument called a hemostat punctures the skin and spreads the tissue. The non-scalpel technique moves tissue to the side, rather than cutting through tissue. While both techniques are effective, the non-scalpel technique causes fewer complications.²
The inner part of the vas deferens, the part that transmits sperm, is about the size of a human hair. The goal of vasectomy is to close this inner channel to prevent sperm from traveling to the prostate and urethra during ejaculation. This can be done using cautery (which uses electricity to heat and scar the tube shut), tiny clips, suture, displacement of one end of the tube apart from the other, or a combination of these.
After vasectomy, there may be absorbable stitches in the skin. These sutures do not need to be removed. It is common to experience a dull ache in the scrotum that radiates to the groin (that is where the nerves travel). For the first few days, the more time spent reclining, with frequent ice packs to the scrotum, the less pain and swelling you will experience. Be aware, young fathers, that for unexplained reasons, small children seem especially apt to hit, jump on, or otherwise contact these sensitive areas. It’s as if there is a Death Star tractor beam attracting young ones to the scrotum for the first few days after vasectomy. After three days, however, one may usually return to normal work and home life. Narcotic pain medicine, if used at all, is usually not needed after the second day.
Ejaculation should be avoided for one week after vasectomy. Other forms of contraception must be used until it is proven that all the sperm are absent. A semen analysis after approximately 15 ejaculations (or after 8-16 weeks, surgeon preference) is required before resuming unprotected intercourse.
The most common complications following vasectomy are bleeding and infection. Thankfully, these are rare and only occur 1-2% of the time. Serious complications are extremely rare. Post vasectomy pain syndrome (pain that persists beyond the normal recovery period) occurs in roughly 1% of men. The risk of pregnancy after successful vasectomy with proven absence of sperm is approximately 1 in 2000.³
FACT: Vasectomy does NOT impair sexual interest or performance.
As described above, the tube that is occluded during vasectomy only carries sperm. Testosterone is the hormone that causes sexual interest and improves erectile ability. Testosterone is produced by the testicle and secreted directly into the bloodstream. This production and secretion are NOT affected by vasectomy. Vasectomy also does NOT increase risk for prostate cancer, heart disease, stroke, hypertension, dementia, testicular cancer,³ or immune-complex diseases such as lupus.¹
FACT: Vasectomy can be reversed.
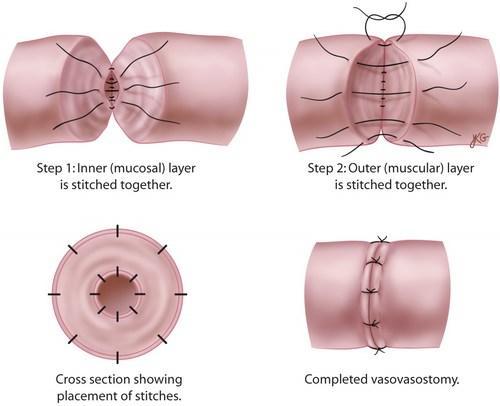
Vasectomy can be reversed to restore fertility. However, this operation is much more involved than a vasectomy. Vasectomy reversal is not commonly covered by insurance and can cost $2,500-5,000. This surgery is often performed under general anesthesia or deep sedation. It is a much more delicate operation that involves reconnecting the hair-sized opening with tiny suture (Figure 2). The opening is so small that a surgical microscope is often used for better visualization. Vasectomy reversal is approximately 50-65% successful. Vasectomy reversal fertility rates are best with a young female partner and when the vasectomy was performed recently. Although vasectomy can be reversed, individuals considering vasectomy should consider this a permanent form of sterilization.
Let’s review the facts: vasectomy is a safe and effective procedure for male sterilization. It is less expensive and safer than female sterilization. Vasectomy does not impair sexual interest or performance. Although vasectomy can be reversed, it should be considered a permanent choice for male sterilization. For these reasons, the “snip-snip” is a snap!
Sources:
1. Shih G, Turok DK, Parker WJ. Vasectomy: the other (better) form of sterilization. Contraception 2011 Apr;83(4):310-5.
2. Cook LA et al. Scalpel versus no-scalpel incision for vasectomy. Cochran Database Syst Rev. 2007 Apr 18;(2):CD004112.
3. http://www.auanet.org/education/guidelines/vasectomy.cfm
Figure 1: Vasectomy: Vas deferens are divided on both sides. (image courtesy of https://www.urologysanantonio.com/vasectomy)
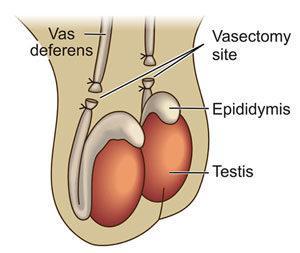
Figure 2: Vasectomy reversal: The small vas deferens opening is sewn back together. (image courtesy of https://www.urology.co.nz/info/vasectomy-reversal)